April 15th – April 22nd 2022
Cannabis and Pets: Clinical Outcomes Results from North American Veterinarians
Cannabis poisoning in pets have increased since legalization, with the most common route of ingestion attributed to edibles.
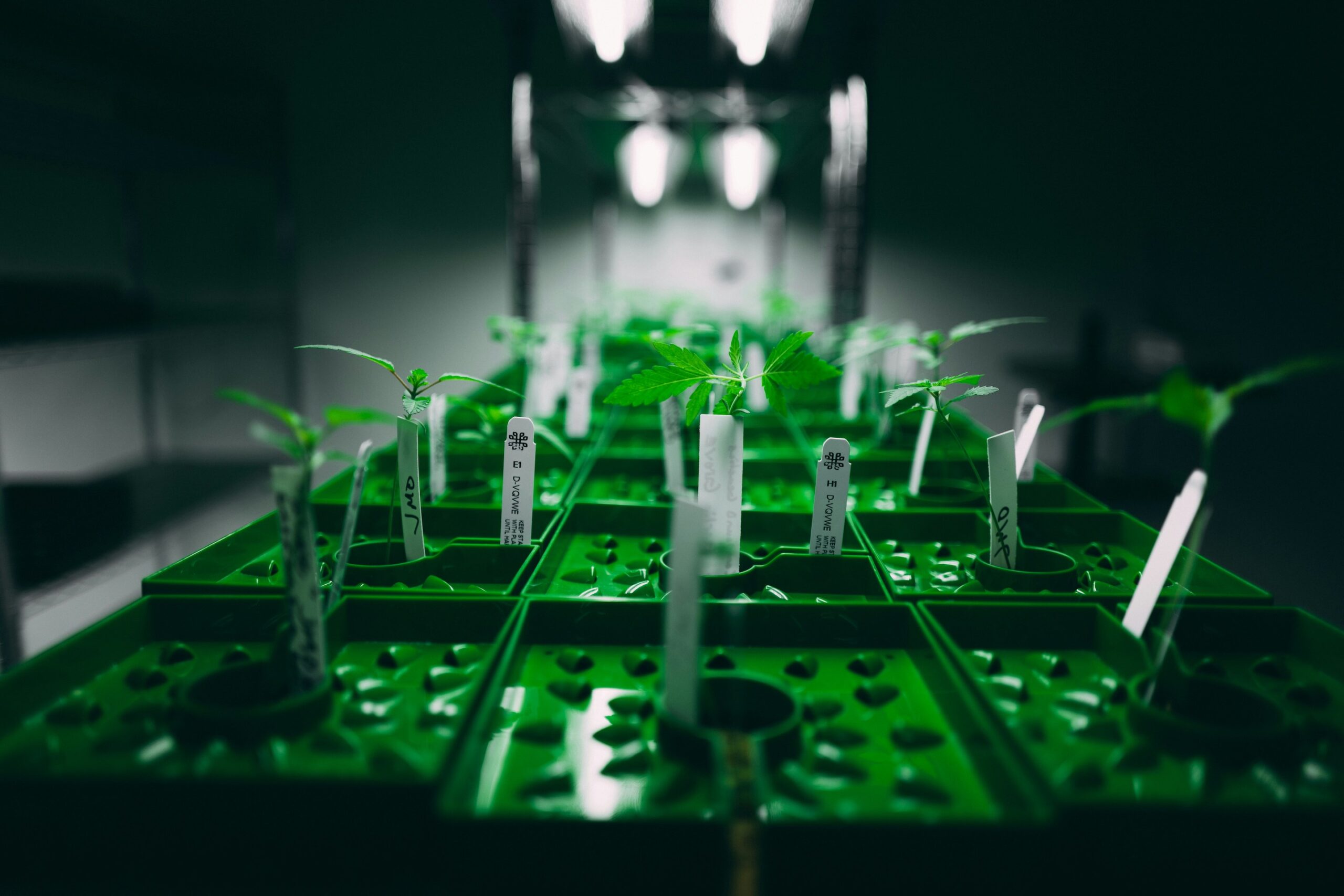
Along with the increasing number of US states legalizing cannabis, studies demonstrating its therapeutic benefits in both animal and human models are on the rise. As such, it is not surprising that accessibility and increased public interest have landed in the field of veterinary medicine. [1] While the sales of cannabis containing products for pets have increased by 1000% between 2016 and 2017, there are limited studies examining the potential outcomes and side effects associated with its use. [2]
Despite the Animal Poison Control Center reporting a 765% increase in calls regarding pets ingesting cannabis in 2019 compared to 2018, outcomes of these incidents remain unknown. [3]
A group of Canadian researchers aimed to gather information via online surveys asking veterinarians regarding any differences in frequency of cannabis toxicoses before and after legalization in Canada, determine any potential clinical signs, and identify whether evidence can support lethality among pets following cannabis consumption. [4]
Between January 2021 and April 2021, they obtained responses from 222 study participants, with the majority based in Canada. Not surprisingly, they found that dogs and cats were among the pets which reported the most cannabis toxicoses, with the numbers increasing in both Canada and the US after 2018. In addition, the most frequently reported clinical signs included urinary incontinence (i.e., inability to control urination), disorientation, and ataxia (i.e., impaired balance or coordination). The most common route of cannabis exposure was ingestion, with edibles followed by dried cannabis being the most suspected cause of toxicosis.
The authors concluded: “There is a need for more sensitive and specific diagnostic tests to diagnose cannabis toxicities, whether to support aggressive decontamination procedures in high-risk patients, or to differentiate between non synthetic cannabis (lethality unknown) and synthetic cannabis (known to be lethal in dogs. As the burgeoning field of medicinal cannabis use in humans and animals continues to grow, fundamental research into the pharmacokinetics, pharmacodynamics, and potential lethality of cannabis in different animal species is also needed to address outstanding research gaps.”
Can Cannabidiol (CBD) Have Anti-Aging Properties?
CBD application led to autophagy induction and neuronal health improvement in C. elegans.
Aging is widely recognized as an inevitable biological process leading to gradual changes and deterioration in most body systems and in all tissues. [5] It is a physiological process mediated by numerous biological and genetic pathways, directly linked to lifespan and are a driving force for all age-related disease states. [6] The effect of aging is mostly observed in the nervous system, with pathological diseases including Alzheimer’s and Huntington’s diseases.
One of the processes that is affected and disrupted during aging is a cellular process called autophagy, defined as the body’s own natural mechanism to remove, and clean out damaged cells. [7] Dysfunctional autophagy has been linked to accelerated aging, and therefore understanding how to induce autophagy may potentially have anti-aging effects.
The cannabis plant is composed of more than 100 phytocannabinoids, with cannabidiol (CBD) being the most investigated non-psychoactive compound, exhibiting to name a few, anti-inflammatory, and antioxidant properties.[8] Recent studies have shown that CBD application in animal models led to increased lifespan and improve health span but the mechanisms behind these effects are not clearly understood. [9],[10]
A group of researchers in Australia used Caenorhabditis elegans (C.elegans) as their animal model to map out these mechanisms. [11] Why use worms you may ask? Well, they can be grown cheaply and in large numbers, have a short life cycle, are transparent (i.e., behavior of individual cells can be followed), their complete genome was published in 1998, and finally are great models to study human diseases, and specifically for studies of neuronal or whole organismal aging. [12]
Using a wide array of experimental techniques, they found that CBD induced neuronal autophagy, promoted autophagic flux in neurons, and improved health span and neuronal morphology associated with aging via the protein sirtuin 1 (SIRT1), known to link the extension of lifespan and age-related cellular mechanisms. [13]
The authors concluded: “Our study provides evidence that CBD contributed to extending lifespan and ameliorating the deterioration of aging-related physical functions in C. elegans… Our results are the first to provide the anti-aging mechanisms of CBD promoting lifespan and ameliorating neuronal aging, which forms a basis for the possible application of CBD in improving neuronal health and longevity.”
CANreduce 2.0: a Web-Based Approach to Decrease Cannabis Use in Individuals with Attention-Deficit Hyperactivity Disorder (ADHD)
This intervention reduced both cannabis use and ADHD scores in individuals with ADHD.
Attention-deficit hyperactivity disorder (ADHD) is a prevalent, chronic, and pervasive childhood disorder characterized by developmentally inappropriate activity level, impulsivity, and inability to sustain attention and concentration. [14] It is one of the most common neurodevelopmental disorders in childhood, with a worldwide prevalence of 5% in children and up to 4% in adults. [15]
While perceived as a safe drug with clinical therapeutic benefits in Western societies, cannabis use in individuals with medical conditions can have a worsening impact. Along those lines, reports show that individuals with ADHD tend to use cannabis more frequently and individuals with cannabis use disorders (CUD) are more common in those with ADHD, suggesting a bi-directional effect of cannabis use to ADHD. [16] In addition, studies have indicated that individuals with ADHD are at a higher risk of using cannabis leading to worsening of ADHD symptoms.[17],[18]
In a previous trial (CANreduce 2.0 study), Amann et al. found that self-guided web-based intervention was able to decrease cannabis use and reduce general anxiety disorder symptoms compared to the control group. [19] While web-based interventions have provided some relief for these individuals, further analysis is needed to determine whether these kinds of interventions can help reduce cannabis use in individuals with ADHD.
The same group of researchers aimed to gain additional insights into whether CANreduce 2.0 can be a beneficial web-based tool to reduce cannabis consumption in individuals with ADHD. [20] This self-help intervention includes motivational interviewing techniques, cognitive behavioral therapy, self-control practices, and social problem-solving.
They found that both individuals with and without ADHD reduced their cannabis use frequency as well as severity of cannabis use and anxiety symptoms. Additionally, and most importantly, individuals with ADHD reported a decrease in their symptoms scores, suggesting this intervention can be beneficial not only to limit cannabis use and to potentially ameliorate their well-being.
The authors concluded: “The CANreduce 2.0 program appeared to benefit both individuals with and without attention deficit/hyperactivity disorder similarly. This web-based program offers a personalized counselling option designed to increase intervention adherence and may provide a viable option to reach cannabis users remotely, including those with attention deficit/hyperactivity disorder, and improve both psychiatric comorbidities and overall condition.”
Can Cannabidiol (CBD) Have Anti-Addiction and Anti-Psychotic Properties?
CBD was able to reduce behavioral sensitization to methamphetamine in rats, a new study reports.
Methamphetamine is a Schedule II powerful stimulant under the Controlled Substances Act (i.e., high potential for abuse and a currently accepted medical use) affecting the central nervous system (CNS). [21] It is known to be a highly illicit drug associated with major physical and mental health problems when used including cognitive and neurological issues with a high risk of drug dependence. [22]
Methamphetamine works by hijacking the brain leading to an increase in the amount of dopamine, a neurotransmitter involved in motivation, and reinforcement of rewarding behaviors. [23] As such, the users keep turning to this drug developing a drug dependence state due to its euphoric effects, sometimes at increased mental and financial costs.
As of today, there are no currently approved treatments for methamphetamine dependence, and as such there is a strong need to establish novel pharmacotherapy strategies.
One of which is the use of cannabis, and most specifically the major non-psychoactive compound cannabidiol (CBD). In the cannabis plant, cannabidiolic acid (CBDA) acts as the natural precursor molecule through which when exposed to light and heat converts to CBD. On one hand, previous animal models studies have suggested that CBD can have anti-craving effects and can potentially reduce motivation to self-administer methamphetamine. [24],[25] On the other hand, limited research is available on CBDA’s potential to act as a drug-craving agent.
Researchers in Australia aimed to study whether CBD or/and CBDA could attenuate methamphetamine-induced sensitization in locomotor hyperactivity in rats. [26] As such, they were subjected to daily injection of methamphetamine or saline for 7 days, followed by 21 days of withdrawal. Then, they were given either CBD or CBDA at different doses and challenged them with methamphetamine followed by locomotor activity.
They found that as opposed to saline pre-treated, rats pre-treated with methamphetamine had increased locomotor activity that was decreased in the CBD but not CBDA group.
The authors concluded: “The present study showed a sensitized locomotor response to METH in male rats pretreated and that CBD, but not CBDA treatment, was able to attenuate hyperlocomotion characteristic of METH sensitization, at pharmacologically effective doses… The data further reinforce the view that CBD might serve as a novel pharmacotherapy for METH-induced addiction and psychosis.”
References:
[1] Vogt NA, Sargeant JM, Stevens CPG, Dunn JN. A survey of veterinary student attitudes concerning whether marijuana could have therapeutic value for animals. PLoS One 2019;14(7):e0219430. DOI: 10.1371/journal.pone.0219430.
[2] Kogan LR, Hellyer PW, Silcox S, Schoenfeld-Tacher R. Canadian dog owners’ use and perceptions of cannabis products. Can Vet J 2019;60(7):749-755.
[3] https://www.aspcapro.org/resource/marijuana-toxicosis-animals, assessed on April 22, 2022
[4] Amissah RQ, Vogt NA, Chen C, Urban K, Khokhar J. Prevalence and characteristics of cannabis-induced toxicoses in pets: Results from a survey of veterinarians in North America. PLoS One 2022;17(4):e0261909. DOI: 10.1371/journal.pone.0261909.
[5] Johnson FB, Sinclair DA, Guarente L. Molecular biology of aging. Cell 1999;96(2):291-302. DOI: 10.1016/s0092-8674(00)80567-x.
[6] Li Z, Zhang Z, Ren Y, et al. Aging and age-related diseases: from mechanisms to therapeutic strategies. Biogerontology 2021;22(2):165-187. DOI: 10.1007/s10522-021-09910-5.
[7] Dikic I, Elazar Z. Mechanism and medical implications of mammalian autophagy. Nat Rev Mol Cell Biol 2018;19(6):349-364. DOI: 10.1038/s41580-018-0003-4.
[8] Mecha M, Feliu A, Inigo PM, Mestre L, Carrillo-Salinas FJ, Guaza C. Cannabidiol provides long-lasting protection against the deleterious effects of inflammation in a viral model of multiple sclerosis: a role for A2A receptors. Neurobiol Dis 2013;59:141-50. DOI: 10.1016/j.nbd.2013.06.016.
[9] Land MH, Toth ML, MacNair L, et al. Effect of Cannabidiol on the Long-Term Toxicity and Lifespan in the Preclinical Model Caenorhabditis elegans. Cannabis Cannabinoid Res 2021;6(6):522-527. DOI: 10.1089/can.2020.0103.
[10] Pandelides Z, Thornton C, Faruque AS, Whitehead AP, Willett KL, Ashpole NM. Developmental exposure to cannabidiol (CBD) alters longevity and health span of zebrafish (Danio rerio). Geroscience 2020;42(2):785-800. DOI: 10.1007/s11357-020-00182-4.
[11] Wang Z, Zheng P, Chen X, et al. Cannabidiol induces autophagy and improves neuronal health associated with SIRT1 mediated longevity. Geroscience 2022. DOI: 10.1007/s11357-022-00559-7
[12] https://www.yourgenome.org/facts/why-use-the-worm-in-research, assessed on April 22, 2022
[13] Salminen A, Kaarniranta K. SIRT1: regulation of longevity via autophagy. Cell Signal 2009;21(9):1356-60. DOI: 10.1016/j.cellsig.2009.02.014
[14] Cormier E. Attention deficit/hyperactivity disorder: a review and update. J Pediatr Nurs 2008;23(5):345-57. DOI: 10.1016/j.pedn.2008.01.003
[15] Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007;164(6):942-8. DOI: 10.1176/ajp.2007.164.6.942
[16] Estevez N, Dey M, Eich-Hochli D, Foster S, Gmel G, Mohler-Kuo M. Adult attention-deficit/hyperactivity disorder and its association with substance use and substance use disorders in young men. Epidemiol Psychiatr Sci 2016;25(3):255-66. DOI: 10.1017/S2045796015000360
[17] Petker T, DeJesus J, Lee A, et al. Cannabis use, cognitive performance, and symptoms of attention deficit/hyperactivity disorder in community adults. Exp Clin Psychopharmacol 2020;28(6):638-648. DOI: 10.1037/pha0000354
[18] Volkow ND, Wang GJ, Telang F, et al. Decreased dopamine brain reactivity in marijuana abusers is associated with negative emotionality and addiction severity. Proc Natl Acad Sci U S A 2014;111(30):E3149-56. DOI: 10.1073/pnas.1411228111
[19] Amann M, Haug S, Wenger A, et al. The Effects of Social Presence on Adherence-Focused Guidance in Problematic Cannabis Users: Protocol for the CANreduce 2.0 Randomized Controlled Trial. JMIR Res Protoc 2018;7(1):e30. DOI: 10.2196/resprot.9484
[20] Ahlers J, Baumgartner C, Augsburger M, et al. Cannabis Use in Adults Who Screen Positive for Attention Deficit/Hyperactivity Disorder: CANreduce 2.0 Randomized Controlled Trial Subgroup Analysis. J Med Internet Res 2022;24(4):e30138. DOI: 10.2196/30138.
[21] https://www.dea.gov/drug-information/drug-scheduling, assessed on April 22, 2022
[22] Mullen JM; Richards JR; Crawford AT (2018) Amphetamine related psychiatric disorders, StatPearls, Treasure Island, FL
[23] https://nida.nih.gov/publications/drugfacts/methamphetamine, assessed on April 22, 2022
[24] Viudez-Martinez A, Garcia-Gutierrez MS, Fraguas-Sanchez AI, Torres-Suarez AI, Manzanares J. Effects of cannabidiol plus naltrexone on motivation and ethanol consumption. Br J Pharmacol 2018;175(16):3369-3378. DOI: 10.1111/bph.14380.
[25] Hay GL, Baracz SJ, Everett NA, et al. Cannabidiol treatment reduces the motivation to self-administer methamphetamine and methamphetamine-primed relapse in rats. J Psychopharmacol 2018;32(12):1369-1378. DOI: 10.1177/0269881118799954.
[26] Umpierrez LS, Costa PA, Michelutti EA, et al. Cannabidiol but not cannabidiolic acid reduces behavioural sensitisation to methamphetamine in rats, at pharmacologically effective doses. Psychopharmacology (Berl) 2022. DOI: 10.1007/s00213-022-06119-3.