February 25th – March 4th, 2022
Medical Cannabis in Flower Form is Now Available in Minnesota
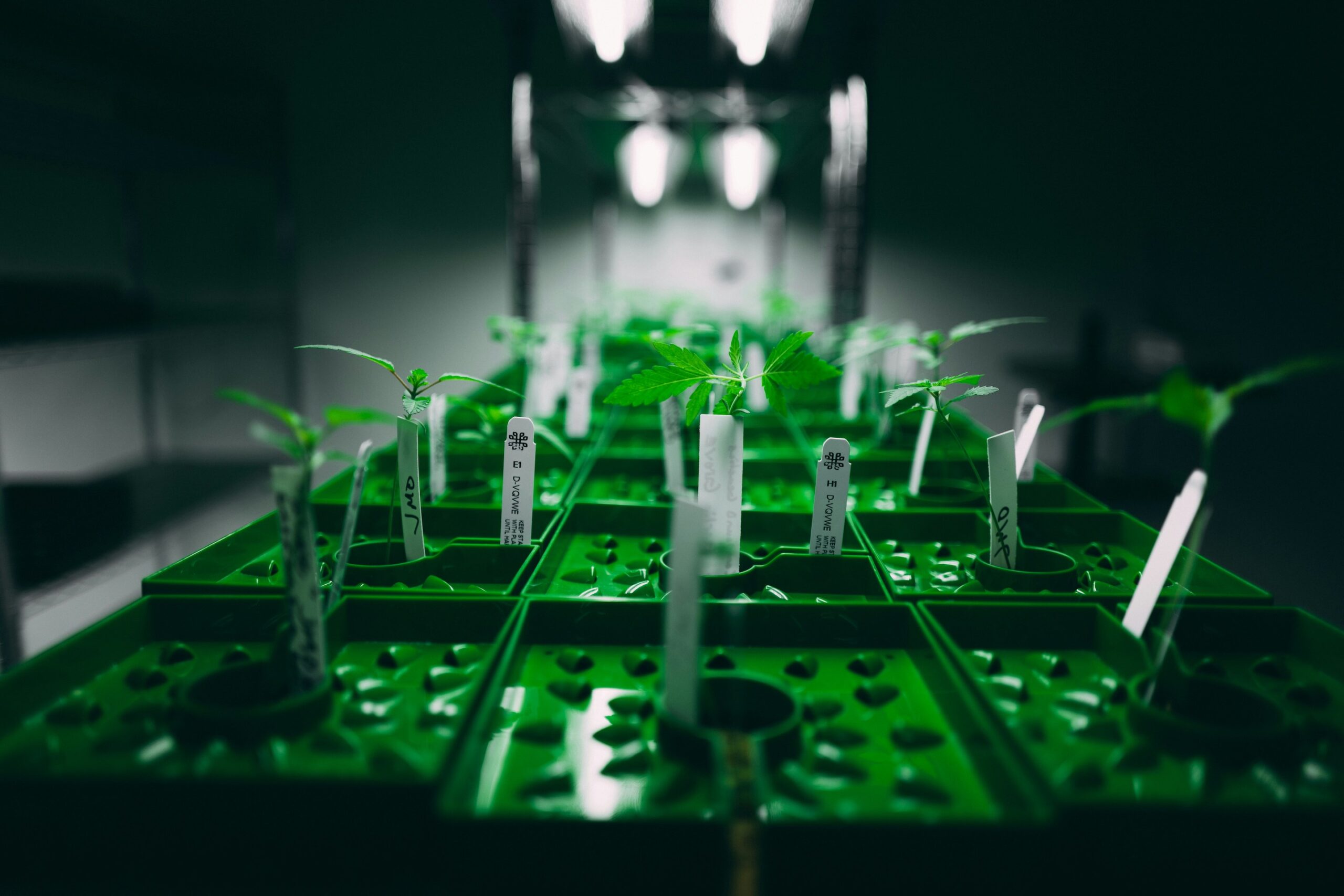
Qualifying Minnesotan medical cannabis patients can now have access to the cannabis flower
On March 1st, 2022, the “North Star State” approved the use of medical cannabis to eligible patients in its dried flower form. [1] Before that, only topical or concentrated cannabis-based products were allowed for these patients. This would be a big help for them due to the high prices of these applications. Chris Tholkes, director of the office of medical cannabis with the health department said: “the number one complaint we have heard from patients over the years is that the price point really. It’s cheaper because it’s not concentrated like wax pens”. [2] As of now, only two dispensaries have received approval to sell dried cannabis.
While several cannabis consumption methods are available, inhalation remains the most common method to consume cannabis. By entering the circulation faster, cannabis consumers can be alleviating their symptoms rapidly and making it easier to manage dosing with inhalation. [3] However, numerous cons are associated with smoking including lung infection and inflammation leading to coughing and shortness of breath as well as risks of addiction. [4]
In 2014, Minnesota approved the use of medical cannabis for patients with qualifying medical conditions including glaucoma, HIV/AIDS, or multiple sclerosis. [5] The state is now discussing to change its status to legalize it for recreational use by 2024, with hope to bring $25 million for the formation of a “cannabis management office”. This would oversee and ensure the safe and responsible legalization for adult cannabis use in the state, according to Governor Theo Keith. [6]
A Journal App to Track Cannabis Consumption
Juva Life launches a new app to self-record cannabis use
Self-medication is the most common method to consume cannabis. It refers to one of two behaviors: 1) the conscious use of nonprescribed medication to treat a condition or 2) the use of an illicit drug to treat a physical or psychological condition consciously or subconsciously. Understanding how one needs to self-medicate is a critical part in properly regulating cannabis consumption. [7]
As such, medical experts recommend using the start low and go-slow approach when identifying the right dosage. In other words, one should start with the smallest dose possible over the course of several days and slowly increase it. To avoid problems with cannabis overuse or misuse, consumers should be guided by an educated physician who specializes in medical cannabis and will discuss the most appropriate and personalized approach. Furthermore, experts recommend using a journal to keep track of previous cannabis use by recording the time and amount of the current product dosage, whether it was taken on an empty stomach, if other medicines were taken along with it and how long it took to feel the effects.
To help digitizing this process, Juve Life, a life science company with pharmaceutical research and development, has launched an application to help track cannabis use for consumers to know how it can affect their health and wellness. [8] More specifically, the application offers a friendly way to document and track their symptoms following cannabis use daily.
Doug Chloupek, CEO and Founder of Java said: “we’re proud to be one of the first and only companies to offer consumers a daily tracking solution that provides them a closer look at how their cannabis use affects their personal health and wellness… One of Juva’s primary goals is to expand our industry’s knowledge of the medicinal effects of cannabis from a scientific perspective. The Journal App provides a personal tracking solution for our customers, and it gives Juva information that compliments the data we collect via our research registry.” [9]
Currently, the company identified two non-cannabinoid compounds, JUVA-019, and JUVA-041, which demonstrate anti-inflammatory properties. [10]
Physiology and Bioenergetics Effects of Cannabidiol (CBD) Administration Following Aerobic Exercise
Understanding how CBD affects athletes’ performances may help them make better use of the compound
The cannabis plant contains more than 500 compounds but ∆9-tetrahydrocannabinol (∆9-THC) and cannabidiol (CBD) are the most studied. While ∆9-THC is associated with euphoric-like effects, increasing attention has shifted towards CBD, the major non-psychoactive phytocannabinoid in the plant. In addition, this is a well-established anti-convulsant with a high therapeutic potential and low safety profile. [11],[12] This molecule is also gaining high interest among athletes who claim it can enhance recovery, improve sleep, and reduce anxiety. [13] Interestingly, the Tokyo 2020 Olympic games became the first of its kind to allow elite athletes to use CBD-based compounds to help them prepare for the competitions. [14] Despite this historic decision, only two randomized, double-blind, placebo-controlled studies have investigated the effects of CBD administration on athletic performance. [15],[16]
A group of researchers at the Lambert Initiative for Cannabinoid Therapeutics at the University of Sydney, aimed to determine the effects of acute, oral CBD treatment on physiological and psychological responses to aerobic exercise. [17] To determine this, nine male endurance-trained runners were recruited and administered CBD or placebo 1h before a run exercise at fixed intensity (run 1) and an incremental run exercise (run 2). Data collected at the end of exercise included respiratory gases (VO2), sweat loss, blood pressure, gastrointestinal comfort, blood sampling and biomarker analyses, and subjective feelings.
They found that CBD administration increased VO2, ratings of pleasure, and blood lactate concentrations during run 1 while also increasing VO2 and respiratory exchange ratio (RER) during run 2. While exercise increased the serum of certain pro-inflammatory markers, CBD also appeared to suppress some of these markers.
Future studies should increase the study sample size, with matching number of men and women as well as considering different CBD doses.
The authors concluded: “these preliminary results suggest that acute, oral CBD treatment has the potential to alter key physiological and psychological responses during aerobic exercise… Further research, involving a larger participant sample and different dosing regimens (e.g., chronic treatment, lower doses), is required to confirm and better understand these initial observations.”
Can Brain Stimulation be Used as a Treatment for Cannabis Use Disorders (CUD) Individuals with Schizophrenia Symptoms?
This method showed promising results in reducing cannabis use in CUD individuals with schizophrenia, a new study finds
Schizophrenia is a complex, chronic mental health disorder characterized by delusions, hallucinations, disorganized speech or behavior, and impaired cognitive ability. [18] It is estimated that 1.5 million US adults have schizophrenia, making it one of the top 15 leading causes of disability worldwide. [19] Individuals with cannabis use disorders (CUD) is a condition in which users develop dependance with increasing cannabis use and can be seen in up to 30% of cannabis consumers. [20] Evidence indicate that cannabis use can worsen psychiatric symptoms and is a risk factor for schizophrenia. [21] Despite some promising therapies being investigated, managing CUD in individuals with schizophrenia is a challenge and novel treatments may shine new lights into treating this population.
One of which is the neuromodulation such as the repetitive transcranial magnetic stimulation (rTMS), a recently developed non-invasive brain stimulation method, producing magnetic field pulses to specific brain regions. While high frequency rTMS has shown promises in reducing drug craving including CUD, additional studies are needed.
Researchers from multiple centers in Canada aimed to investigate the effect of five days a week for four weeks of active rTMS treatment vs. sham (no excitability) applied on the dorsolateral prefrontal cortex (DLPFC), a brain region involved in general executive functions, inhibition, planning, and working memory, in CUD individuals with schizophrenia. [22],[23],[24] Outcomes included cannabis craving/withdrawal, psychotic symptoms, and cognition.
19 participants (n=9 active vs. n=10 for sham) were enrolled in the randomized, double-blind, parallel group, sham-controlled study. Results showed that the active group displayed a greater reduction in self-reported cannabis use as well as improvement in attention. A trend in craving reduction was also noted in the active group but it was not statistically significant compared to the sham group. Study limitations included small sample size and male dominated cohort.
The authors concluded: “these preliminary findings provide important insights into the therapeutic potential of rTMS to the DLPFC in people with co-occurring schizophrenia and CUD.”
References
[1] https://www.health.state.mn.us/people/cannabis/patients/smokablefaq.html#purchase1, assessed on March 2nd, 2022
[2] https://www.mprnews.org/story/2022/03/01/flowering-medical-marijuana-now-available-in-minnesota, assessed on March 2nd, 2022
[3] Huestis MA, Henningfield JE, Cone EJ. Blood cannabinoids. I. Absorption of THC and formation of 11-OH-THC and THCCOOH during and after smoking marijuana. J Anal Toxicol 1992;16(5):276-82. DOI: 10.1093/jat/16.5.276
[4] Tashkin DP. Marijuana and Lung Disease. Chest 2018;154(3):653-663. DOI: 10.1016/j.chest.2018.05.005
[5] https://www.revisor.mn.gov/laws/2014/0/Session+Law/Chapter/311/, assessed on March 2nd, 2022
[6] https://www.fox9.com/news/marijuana-legalization-in-minnesota-gov-walz-pushes-for-legalization, assessed on March 2nd, 2022
[7] Suh JJ, Ruffins, S., Robins, C.E., Albanese, M.J, Khantizian, E.J. Self-medication hypothesis – connecting affective experience and drug choice. APA 2008;25 (3)(518-532). DOI: 10.1037/0736-9735.25.3.518.
[8] https://juvalife.com/juva-life-launches-journal-app-offering-personal-health-and-wellness-tracking-for-cannabis-patients/, assessed on March 2nd, 2022
[9] https://juvalife.com/juva-life-launches-journal-app-offering-personal-health-and-wellness-tracking-for-cannabis-patients/, assessed on March 2nd, 2022
[10] https://juvalife.com/research/, assessed on March 2nd, 2022
[11] https://www.accessdata.fda.gov/drugsatfda_docs/nda/2018/210365Orig1s000Approv.pdf, assessed on March 3rd, 2022
[12] Larsen C, Shahinas J. Dosage, efficacy and safety of Cannabidiol administration in adults: a systematic review of human trials. J Clin Med Res. 2020; 12:129–41
[13] Kasper AM, Sparks SA, Hooks M, Skeer M, Webb B, Nia H, Morton JP, Close GL. High prevalence of Cannabidiol use within male professional Rugby Union and League Players: a quest for pain relief and enhanced recovery. Int J Sport Nutr Exerc Metab. 2020; 30:1–8
[14] https://www.forbes.com/sites/ajherrington/2021/07/21/cannabis-takes-the-world-stage-at-the-tokyo-olympics/?sh=f0522334cb7f, assessed on March 3rd, 2022
[15] Cochrane-Snyman KC, Cruz C, Morales J, Coles M. The effects of Cannabidiol oil on noninvasive measures of muscle damage in men. Med Sci Sports Exerc. 2021; 53:1460–772
[16] Isenmann E, Veit S, Starke L, Flenker U, Diel P. Effects of Cannabidiol supplementation on skeletal muscle regeneration after intensive resistance training. Nutrients. 2021; 13:3028
[17] Sahinovic A, Irwin C, Doohan PT, et al. Effects of Cannabidiol on Exercise Physiology and Bioenergetics: A Randomised Controlled Pilot Trial. Sports Med Open 2022;8(1):27. DOI: 10.1186/s40798-022-00417-y
[18] Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: overview and treatment options. P T 2014;39(9):638-45. (https://www.ncbi.nlm.nih.gov/pubmed/25210417)
[19] Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017 Sep 16;390(10100):1211-1259
[20] Budney AJ, Roffman R, Stephens RS, Walker D. Marijuana dependence and its treatment. Addict Sci Clin Pract 2007;4(1):4-16. DOI: 10.1151/ascp07414
[21] Patel, R. et al. Cannabis use and treatment resistance in first episode psychosis: a natural language processing study. Lancet 385, S79 (2015)
[22] Bidzinski KK, Lowe DJE, Sanches M, et al. Investigating repetitive transcranial magnetic stimulation on cannabis use and cognition in people with schizophrenia. NPJ Schizophr 2022;8(1):2. DOI: 10.1038/s41537-022-00210-6
[23] Brunoni, A., and Vanderhasselt, M.-A. (2014). Working memory improvement with non-invasive brain stimulation of the dorsolateral prefrontal cortex: a systematic review and meta-analysis. Brain Cogn. 86, 1–9. doi: 10.1016/j.bandc.2014.01.008
[24] Hart, H., Radua, J., Nakao, T., Mataix-Cols, D., and Rubia, K. (2013). Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication and age effects. JAMA Psychiatry 70, 185–198. doi: 10.1001/jamapsychiatry.2013.277