Why we think it’s important
This study is important because it helps us understand what happened to hospitalizations when Canada made nonmedical cannabis legal. It shows that while there was initially a decrease in hospitalizations right after the law changed, later on, when more cannabis was available, there was an increase in health issues related to cannabis.
Introduction
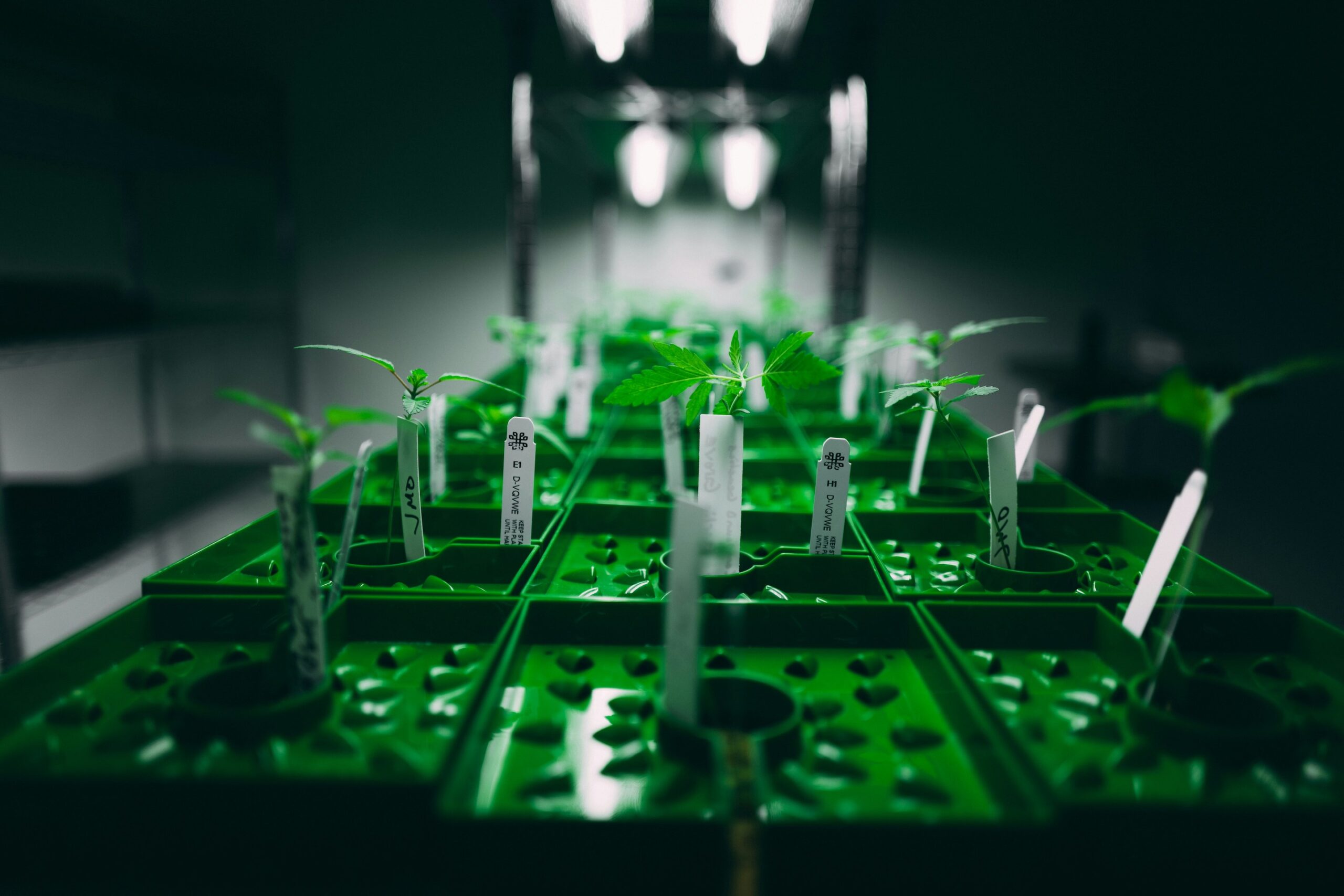
In October 2018, Canada took a significant step by legalizing nonmedical cannabis for adult use. This decision prompted a closer look at the potential health implications of widespread cannabis availability. A recent study, “Changes in Cannabis-Attributable Hospitalizations Following Nonmedical Cannabis Legalization in Canada,” investigates the impact of this legalization on hospitalization rates across the country.
Understanding the Study
The study involved a comprehensive analysis of hospitalization data from Canada’s four most populous provinces: Ontario, Quebec, Alberta, and British Columbia. Covering a 7-year period from January 2015 to March 2021, the study aimed to uncover changes in hospitalizations due to cannabis before, during, and after legalization.
Key Findings
The research revealed a nuanced pattern in cannabis-related hospitalizations. Initially, there was a surge in hospitalizations leading up to the legalization, attributed to increasing cannabis use and changing societal norms. Strikingly, the study found that the immediate post-legalization period, marked by restricted product availability and store access, was associated with a modest decrease in hospitalizations. However, the scenario shifted during the subsequent phase of broad commercialization, coinciding with the onset of the COVID-19 pandemic, leading to a notable increase in cannabis-related hospitalizations.
Variation Across Provinces
One notable aspect of the study was the provincial variation in the impact of cannabis legalization. Provinces with less mature legal markets experienced the greatest decline in hospitalizations immediately following legalization. However, during the commercialization phase, the provinces with more significant legal cannabis sales growth observed a substantial increase in hospitalizations. This emphasizes the influence of regional policies and market maturity on the outcomes of cannabis legalization.
Types of Hospitalizations and Concerns
The study also delved into specific types of cannabis-related hospitalizations, revealing that cannabis-induced psychosis saw the largest relative increase. This finding raises concerns about the potential long-term impact of cannabis legalization, particularly concerning mental health issues.
Implications for Policy
The findings of this study offer crucial insights for policymakers. The initial period of tight control over cannabis products and limited store access appeared to have a positive impact on hospitalization rates. However, the subsequent phase of market expansion and product proliferation saw a concerning rise in cannabis-related health issues. As jurisdictions around the world contemplate cannabis legalization, this research suggests that careful regulation and monitoring of product types and store access may mitigate potential risks associated with increased cannabis availability.
Final Thoughts
In navigating the waves of cannabis legalization, Canada’s experience provides valuable lessons. The study underscores the importance of adopting a cautious approach to market expansion and product diversification, especially in the context of potential health risks associated with cannabis use. As the cannabis landscape continues to evolve, ongoing surveillance efforts and adaptive policies will be essential to strike a balance between access and public health.
“Changes in Cannabis-Attributable Hospitalizations Following Nonmedical Cannabis Legalization in Canada.” (D. T. Myran, et al., JAMA Netw Open, 2023)
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2810194?resultClick=1